Staphylococcus below a cover glass- Makes the difference
Greetings
Clinical conditions:
Photo 1: Gram-positive Staphylococcus aureus, from a laboratory culture (Source), and Staphylococcus aureus in culture (Source)
1. Methicillin
2. Cefazolin
3. Cefuroxime
4. Erythromycin
5. Clindamycin
Micrococcus species:
 Melter O, Tkadlec J, & Sedláček I (2012). A simple and cost-effective cover-glass test for the differentiation between staphylococci and micrococci in clinical laboratory. Journal of microbiological methods, 89 (3), 213-5 PMID: 22446099
Melter O, Tkadlec J, & Sedláček I (2012). A simple and cost-effective cover-glass test for the differentiation between staphylococci and micrococci in clinical laboratory. Journal of microbiological methods, 89 (3), 213-5 PMID: 22446099
Further Reading:
In the modern day of Laboratory diagnostics, people rely more on hifi techniques like PCR, DNA sequencing or even a microarray analysis for even the most common pathogen. The fact is it doesn't have to be so. Even to this date despite robotics and digtalization of most of the laboratory set up, a simple gram stain microscopy and simple biochemical tests such as catalase and oxidase is invaluable. And i don't think anyone would counter state it.
This blog is about a paper published in "Journal of Microbiological Methods". The article is entitled "A simple and cost-effective cover-glass test for the differentiation between staphylococci and micrococci in clinical laboratory" by Oto Melter etal (Link to the article).
Staphylococcus:
Staphylococcus is a well studied bacterial pathogen. Rosenbach provided the first taxonomic description of Staphylococcus in 1884 when he divided the genus into Staphylococcus aureus and Staphylococcus albus. The genus Staphylococcus now belongs to the broad Bacillus–Lactobacillus–Streptococcus cluster consisting of Gram-positive bacteria that have a low G + C content of DNA. The closest relatives of staphylococci are the macrococci. They are also related to salinicocci, enterococci, planococci, bacilli and listerias on the basis of partial oligonucleotide sequencing of 16S rRNA and rDNA. Taxonomically, the genus Staphylococcus is in the bacterial family Staphylococcaceae, which includes three lesser known genera, Gamella, Macrococcus and Salinicoccus.
Staphylococcus is a well studied bacterial pathogen. Rosenbach provided the first taxonomic description of Staphylococcus in 1884 when he divided the genus into Staphylococcus aureus and Staphylococcus albus. The genus Staphylococcus now belongs to the broad Bacillus–Lactobacillus–Streptococcus cluster consisting of Gram-positive bacteria that have a low G + C content of DNA. The closest relatives of staphylococci are the macrococci. They are also related to salinicocci, enterococci, planococci, bacilli and listerias on the basis of partial oligonucleotide sequencing of 16S rRNA and rDNA. Taxonomically, the genus Staphylococcus is in the bacterial family Staphylococcaceae, which includes three lesser known genera, Gamella, Macrococcus and Salinicoccus.
Staphylococcus aureus has a large set of virulence factors in its armory. The most important adhesion factors involved in colonizing and subsequent skin infections are- Fibronectin-binding proteins A and B, Collagen-binding protein (Cna), Biofilm associated protein (Bap), Elastin-binding protein (EbpS), Map/Eap, Extracellular matrix-binding protein homologue (Ehb) and many more. It also produces exotoxins such as secrets several cytolytic toxins such as α-hemolysin, β-hemolysin, γ-hemolysin, leukocidin, and Panton-Valentine leukocidin (PVL). It can also produce additional group of exotoxins, which include the toxic shock syndrome toxin-1 (TSST-1), the staphylococcal enterotoxins (SEA, SEB, SECn, SED, SEE, SEG, SEH, and SEI) and the exfoliative toxins (ETA and ETB). (Click here for a reference). In addition to all the above, SpA is shown to be an important central virulence determinant. (S. Bronner et al; click here)
Clinical conditions:
Impetigo (It is also known as school sores) is a superficial bacterial skin infection which is most common among pre-school children. It is of 2 types- Impetigo contagiosa and bullous impetigo. The former type is seen as a result of infection and the latter is usually an immunological complication. Cellulitis is a diffuse inflammation of connective tissue with severe inflammation of dermal and subcutaneous layers of the skin. Erysipelas is the term used for a more superficial infection of the dermis and upper subcutaneous layer that presents clinically with a well defined edge. Erysipelas and cellulitis often coexist, so it is often difficult to make a distinction between the two. Folliculitis refers to the infection and its inflammation. Boil (or furuncle) is a skin disease caused by the infection of hair follicles, resulting in the localized accumulation of pus and dead tissue. Suggested risk factors for impetigo include: household crowding, inadequate access to water, heat and humidity, lack of education, and inadequate implementation of adequate personal hygiene.
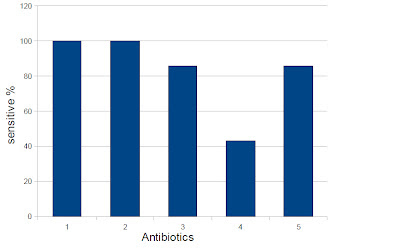
Previously we studied Community acquired Staphylococcus aureus (unpublished data), and its antibiotic sensitivity pattern was as follows.
1. Methicillin
2. Cefazolin
3. Cefuroxime
4. Erythromycin
5. Clindamycin
Micrococcus species:
Micrococcus are genus of bacteria in the Micrococcaceae family, often present as commensals in the skin flora. They are usually recovered in skin culture along with other bacteria. The commonly encountered species include M. luteus; M. lylae; M. roseus etc. They are differentiated from the staphylococcus species by modified oxidase test, susceptibility to furazolidone and lysostaphin, glucose fermentation, acid production from glycerol and growth in Mannitol salt agar. (For details click here).
So, what is this paper about?
The paper is about a simple cost effective differentiation methodology, between pathogenic Staphylococcus and Micrococcus (and related genera such as Dermacoccus, Kytococcus, and Kocuria). The cover glass test, is carried out by using sterile cover-glass which is placed with a pair of sterile tweezers onto a heavily inoculated area of the Columbia blood agar plate with bacterial culture. After overnight incubation at 37 °C, the plate is checked for pigmented colonies or bacterial biomass underneath the cover glass.
Photo 2: Cover-glass (Source)
The growth of staphylococcal colonies was interpreted as weakly positive (+), moderately positive (++) or strongly positive (+++) depending on bacterial growth alteration. (Considered strongly positive if it is an unaffected growth). A negative result will mean that the strain is not able to grow beneath the coverslip.
The test was found to be positive for the staphylococcus (with a few exceptions) and negative for Micrococcus. The way this test makes sense is because staphylococci are facultatively anaerobic and Micrococci are aerobic.
As per i see it, the test is seriously simple enough to perform and cost effective. Many such tests can be carried in a single culture plate. But, I still would recommend that the Modified oxidase test which gives the same result with similar accuracy should be a better bet, because the results are much faster. However, this test can be of academic interest.
*(I didn't use any pictures or tables from the article, owing to copyright issues.) For a full length detail you have to read the article which actually is behind a pay-wall.
Further Reading:
1. Staphylococcus Aureus Diagnosis. (Link)









Comments
Post a Comment